Hi there!
In the previous articles, we saw how atherosclerosis can cause damage to the arteries, developing cardiovascular disease.
We have seen the myocardial infarction yet and today we’ll have a deeper look into peripheral artery disease (PAD).
What is PAD?
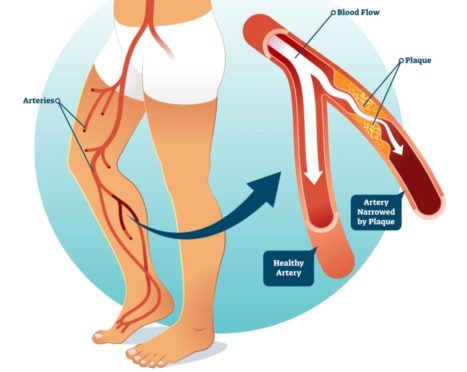
PAD is similar to coronary artery disease: it is caused by stenosis and occlusions of the arteries that carry blood from the heart to other parts of the body.
PAD can occur in any blood vessel, affecting more commonly the legs.
The major risk factors for PAD are as follows:
- Older age: the risk raises above 60 years old;
- Family history and genetics: gene variations and the presence of blood vessels disease, stroke or heart disease can increase the risk of PAD;
- Lifestyle habits: smoking, physical inactivity, unhealthy diet and stress over time can help to buildup a fatty plaque in leg arteries;
- Medical conditions: obesity, diabetes, high blood pressure, high blood cholesterol and high blood triglycerides.
The most frequent clinical manifestation is the intermittent claudication, which is a pain in one or both lower limbs that appears during physical activity and usually goes away after a few minutes when legs are at rest.
Other signs and symptoms can include numbness, weakness, cramping, heaviness, hair loss, shiny and cold skin, sores and ulcers in the legs or feet.
The symptoms of PAD often develop slowly, but if they get suddenly worse, it could be a sign of a serious problem requiring immediate treatment.
If PAD isn’t adequately treated, it can induce serious complications such as angina, coronary heart disease, stroke or heart attack.
Can physical exercise be considered helpful for PAD?
Patients with PAD have a significant functional impairment. Evidence suggests that regular exercise helps to reduce PAD symptoms and complications improving the ability to walk and carry out daily activities. Particularly, physical exercise can offer different advantages:
- Increases blood flow because of increased capillary number and improved vasodilatation;
- Promotes the redistribution of blood flow;
- Reduces viscosity of blood;
- Increases the concentration of oxidative enzymes in skeletal muscle;
- Improves the efficiency of walking economy and oxygen uptake;
- Increases strength.
One of the best exercises you can do is walking. It’s recommended to walk as long as you can before the symptoms of pain become intolerable. Then, stop and stretch or walk slower until the pain disappears and begin walking again until the pain returns. The duration of the training session should be made of 30 minutes of walking in total. Every 1-2 week you should increase duration achieving 50 minutes of walking in total. Frequency is set at 3 to 5 times per week.
What can I do if a severe intermittent claudication does not let me able to walk?
Don’t worry!!
Other exercise methods have also been studied and have shown to have some efficacy in improving walking outcomes in patients with PAD. These strategies include:
Aerobic arm and leg cycling exercise training: walking can be associated, especially if the patient has difficulty to walk (for example due to the presence of ulcers, severe claudication, etc.), to the arm ergometer or to the exercise bike. These exercises, involving many muscle groups, allow to obtain an improvement of the cardiovascular and systemic apparatus, guaranteeing a better impact on the walk.
Partitioning of training: to delay intermittent claudication you can alternate one leg at a time on the bike or one upper limb at a time on the arm ergometer; you can do several short sessions of training (for example one in the morning and one in the evening); or use a circuit training to guarantee also 30 continuous minutes of physical exercise but alternating the muscle groups (upper limbs and lower limbs).
Resistance training: you can use bands, dumbbells, weight machine or bodyweight exercise to perform 3 sets of 8 repetitions for 7 different muscle groups at an intensity of 30-60% of 1-repetition maximum.
References
Peripheral Artery Disease (2020). National Heart, Lung, and Blood Institute;
Diane Treat-Jacobson et al. (2019). Optimal Exercise Programs for Patients With Peripheral Artery Disease: A Scientific Statement From the American Heart Association. Circulation, 139: e10–e33.
Edited by
Dott. Luca Rotundo


Commenta con Facebook